AI for Eligibility Verification: A Guide for Patient Access & RCM Teams

In U.S. healthcare, front desk staff are often asked to juggle ringing phones, a line of patients, and a dozen browser tabs.
Somewhere in that chaos, someone needs to confirm insurance eligibility & benefits for every single patient. Is the plan active? What’s the copay? How much deductible remains? Is prior auth required?
In theory, it’s a “quick check.” In practice, it’s a nonintuitive multi-step process that requires scrutiny. Learn how practices are transforming this crucial workflow from an underserved current state to a scalable future powered by the latest AI technology like large language models (LLMs) and AI agents.
A Glimpse at AI’s Impact: From 12 Minutes to 40 Seconds
Eligibility verification before AI: A scheduler toggles through payer portals, waits on hold, and decodes EDI 271s -- if they’re lucky, an average of 12 minutes are used up for one patient (no downstream rework is required).
After strategically adding AI: The scheduler clicks once. The AI agent verifies eligibility, calculates copay, and writes results directly into the EHR. The estimate refreshes automatically before the visit. No portals, no calls, no errors.
Key Benefits of AI for Eligibility:
- Verify patient eligibility & benefits in seconds with an AI agent that reads and interprets complex payer data
- Auto re-verify in real-time before the visit and refresh cost estimates when coverage or deductibles change
- Turn payer data into actions: update EHR fields, notify patients, and flag prior authorization needs automatically
- Route only true exceptions to staff -- with context, history, and suggested next steps
- Collect more out-of-pocket (OOP) dollars upfront with confidence, prevent denials, and give your front desk staff hours back every day
The difference isn’t just time saved; it’s predictability. Staff stay focused on patients, check-in lines move, and revenue teams see cleaner claims downstream.
Eligibility Verification Today
Insurance eligibility today is manual, fragmented, and costly. Staff are overwhelmed, Patients can get mixed messages, claims inherit errors, and revenue ultimately suffers under overburdened staff. Here’s how a typical eligibility check unfolds today upon a patient booking:
- Find the patient and policies in the EHR/PM; confirm spelling, date of birth (DOB), subscriber/member ID, and plan version.
- Submit a clearinghouse eligibility check (X12 EDI 270 request → EDI 271 response) or open a payer portal. Some EDIs are not clear on which information applies to which policy, and policies frequently change.
- Call the payer when the response is partial/unclear (for example, is prior auth required?); wait on hold; repeat details to multiple reps.
- Screenshot or copy/paste fragments of coverage into a note; try to decode accumulators (“deductible met?” “OOP remaining?”).
- Do it again next month because benefits can change between scheduling and day of service.
These excessively manual efforts amount to a significant cost. Our provider partners report an average of 12 minutes of staff time required for each verification, which we have calculated at $3 to $10 of overhead. This cost typically applies for every single visit by every single patient. Bottom line: it impacts both your margin and your scalability.
Moreover, every manual step is a chance for small errors that create big problems later: from a transposed member ID, selecting the wrong plan year, missing a specialty-specific benefit, overlooking an authorization requirement, or misunderstanding an accumulator that resets on the first of the month. None of these mistakes feel dramatic in the moment -- but accuracy here determines patients’ trust in your estimates and whether your claim gets paid or denied.
Eligibility is Inefficient With Clearinghouses and EHRs
Most practices move eligibility over standard X12 270/271 via a clearinghouse. You’ll see it in two flavors: batch (send a file overnight, get 271s back later) and real-time (fire a single 270 during scheduling or check-in and receive a response in seconds). These rails cast a wide net -- broad payer coverage, auditability, predictable uptime -- and they’re the backbone of day-to-day verification.
But rails aren’t the whole ride. Clearinghouse responses can be shallow or inconsistent: some payers return little beyond “active coverage” and a generic copay, skipping the nuance that actually drives estimates and clean claims (visit caps, modality-specific benefits, reliable auth indicators).
Each payer also structures the 271 differently, so without a normalization layer, your team is still translating fields by hand. Cadence is another trap: batch results can go stale by day of service, and even real-time checks need T-48/T-24 re-verification to catch accumulator movement and last-minute plan changes. Edge cases -- secondary coverage/coordination of benefits (COB), carve-outs, plan-year rollovers -- often come back partial or unknown, forcing staff to portals or phones.
Layer on the EHR reality: most systems feature a “Check Eligibility” button that simply passes the request to the clearinghouse and drops the raw 271 back into a note or data file. Out of the box, that means data retrieval without interpretation.
Specialty nuances and plan limits rarely map to default fields; accumulators like deductible, out-of-pocket max, and met % are left for staff to decode; the check is one-and-done with no built-in re-verification cadence; exceptions stall because there’s no automated retry, source switching, nor guided next step; and downstream actions don’t fire -- no auto-refreshed estimates, no plain-language patient summaries with portal-optional pay, no structured writing into the places that scrubbing, auth screening, and dashboards actually read.
Put simply: the clearinghouse can deliver a response and the EHR can show it, but neither is designed to decide and act.
The Costs of Manual Burdens, Errors, and Exceptions
A Lagging Process
Manual eligibility is a 12-minute bottleneck that taxes patient access, revenue, and morale. Multiply those 12 minutes, or the associated $3 to $10, by even a modest daily volume and you’re consuming vast bandwidth and margin on portal hopping and phone trees instead of patient care.
This drag is highly visible, as it shows up in waiting rooms. Patients sit longer while front-desk teams chase payers, which erodes trust at the first touchpoint -- right when you’re confirming coverage and discussing money. For walk-ins and same-day care, every extra minute compounds downstream: schedules back up, providers idle, and clinical time is forced to accommodate administrative lag.
Finally, there’s the human toll. Constant context switching -- portals, phone queues, cryptic codes, and tough conversations about surprise balances -- drives burnout and turnover. Replacing experienced patient access staff is expensive, and the institutional knowledge that walks out the door increases the odds of future errors.
Where Mistakes Happen
Most eligibility errors are boring, human, and totally predictable. They start with data entry: a transposed member ID, an outdated plan version, or the subscriber/DOB entered under the wrong person. Then comes interpretation -- benefits jargon invites mix-ups like treating coinsurance as a copay or confusing deductible with out-of-pocket max.
Scope mistakes creep in when specialty limits, visit caps, carve-outs, or a prior auth requirement are buried in fine print and never make it into the estimate. And finally, there’s timing: if eligibility is verified at scheduling and never again, accumulators move and plans flip between booking and the visit -- resulting in inaccurate estimates and denials.
Downstream Consequences
Up front, trust erodes first. If the number you quoted doesn’t match the bill, patients hesitate, dispute, or delay payment until the explanation of benefits (EOB) arrives. Any extra friction -- forcing a portal login, no simple payment plan -- turns “willing to pay” into “will pay later,” which often becomes “won’t pay.”
Downstream, claims performance suffers: the wrong plan type or a missed prior auth becomes an avoidable denial. Even when recoverable, you’ve added days to cash and soaked up staff time. Operationally, the front desk drifts into call-center mode -- portal hopping, hold music, copy/paste -- while check-in lines grow, providers start late, and leaders get only a partial picture because the details live in screenshots and free-text notes rather than structured fields.
What It Costs
Higher patient A/R: if 15% of visits are inaccurate and those visits see 20% lower in-person collection on a $300 average responsibility, you would see $9,000 in additional A/R each month per 1,000 visits.
Denials tell a similar story: with a 20% denial rate, about a quarter to a third tied to registration or eligibility, and a modest 25% prevention, you avoid ~12–14 denials per 1,000 claims. At ~$45 to rework each denial (setting-dependent), addressing the root causes of these denials can reduce your cost to collect and boost the bottom line with fewer write-offs.
Labor adds up, too: if manual/portal checks take 4–12 minutes longer than a clean pass, and you run 2,000 checks a month at a $30 loaded hourly rate, reclaiming just eight minutes per check is roughly $8,000 in monthly capacity returned to the team.
The Hidden Costs Most Teams Forget
There are softer -- but very real -- hits that compound over time. Once a patient’s confidence is dented, subsequent payments and reviews get harder. Last-minute prior auth surprises force reschedules that ripple through provider utilization and patient satisfaction. And the human cost is real: high-empathy front-office staff burn out faster when their day is dominated by portals and hold queues instead of human conversations.
Where Time is Better Spent
Freeing the team from eligibility means they can do the work only people can do. Up front, that means driving opportunity for your practice to recover more revenue: explaining plain-language estimates, gaining consent for autopay, and walking through patient financing.
With the baseline of automated eligibility verification, teams can focus human judgment on the 10–20% of true exceptions that AI can’t resolve, which lowers average handle time and escalations. And it means keeping check-in moving so providers start on time and patient experience improves. It also means patient access teams can dedicate time to other human-required work like receiving and processing faxes, running prior authorizations, and providing top-tier service to patients.
There is a Better Way: Orchestration With AI
AI can now function as the brain between your EHR/PM, clearinghouse, payers, and patients. In a basic version of automation, it routes requests and formats responses. In the ideal state, which incorporates technology like LLMs and agentic AI, it behaves like a goal-directed teammate: it initiates data transactions, reasons about incomplete data, and then acts -- quietly closing loops so people don’t have to, but escalating when needed.
A canonical benefits model (the “single source of truth”).
Raw payer payloads are messy and inconsistent. The AI leverages LLM functionality to normalize each 271 response into a structured benefits object -- plan type, copay, coinsurance, accumulators (met/remaining), OOP max, plan limits by modality, and an authorization indicator -- and agentically writes those fields to the correct places in your EHR/PM. No more screenshots or sticky-note band-aids; estimates, auth screening, and claim scrubbing all read from the same clean record.
Exception automation that actually helps.
Partial or unknown responses don’t stall; they branch. The AI agent interprets reason codes, retries with backoff, switches data sources if needed, and assembles a human-ready packet only when judgment is required: payer, timestamps, what was attempted, the raw snippet, and a suggested next step. Result: staff time shifts from scavenger hunts to quicker, decisive resolution.
Acting on data, not just storing it.
Once benefits are normalized, the system does things: it updates the estimate, generates a plain-language summary, and sends a portal-optional pay link and 60-second plan options. If auth is likely, it flags it upstream and can kick off the auth workflow.
Evidence you can rely on.
Every interaction leaves a trail: raw 271, transforms, decisions, messages sent, fields written. During audits or appeals, you can show exactly what was known, when, and why the system took a given action.
Learning over time.
Closed cases feed the loop. If a payer starts hiding an auth hint in a new place, the model adapts. If certain AAA codes correlate with successful API fallbacks, the policy optimizes. Over weeks, exception volume shrinks and first-pass success climbs because the system actually gets better.
Guardrails and compliance built-in.
PHI stays encrypted in transit and at rest; rate-limit and backoff policies prevent lockouts; messages are 10DLC-safe and consent-aware; and every EHR write is idempotent with rollback semantics. The AI proposes, but you retain control -- thresholds for auto-actions are transparent and adjustable.
Vendor Evaluation Checklist: What to Ask Before Choosing an AI Eligibility Partner
- Normalizes 271 into structured EHR fields
- Supports T-48/T-24 re-verification and auto estimate refresh
- Handles secondary/COB, carve-outs, and plan-year rollovers
- Provides exception packets with timestamps, reason codes, next step
- Fully SOC 2, HITRUST, and HIPAA compliant
- Consent-aware, 10DLC-safe patient messaging
- Idempotent, auditable writes (who/what/when/why)
- Multilingual summaries + accessibility built in
- Transparent service-level agreements (SLAs) and payer fallback policies
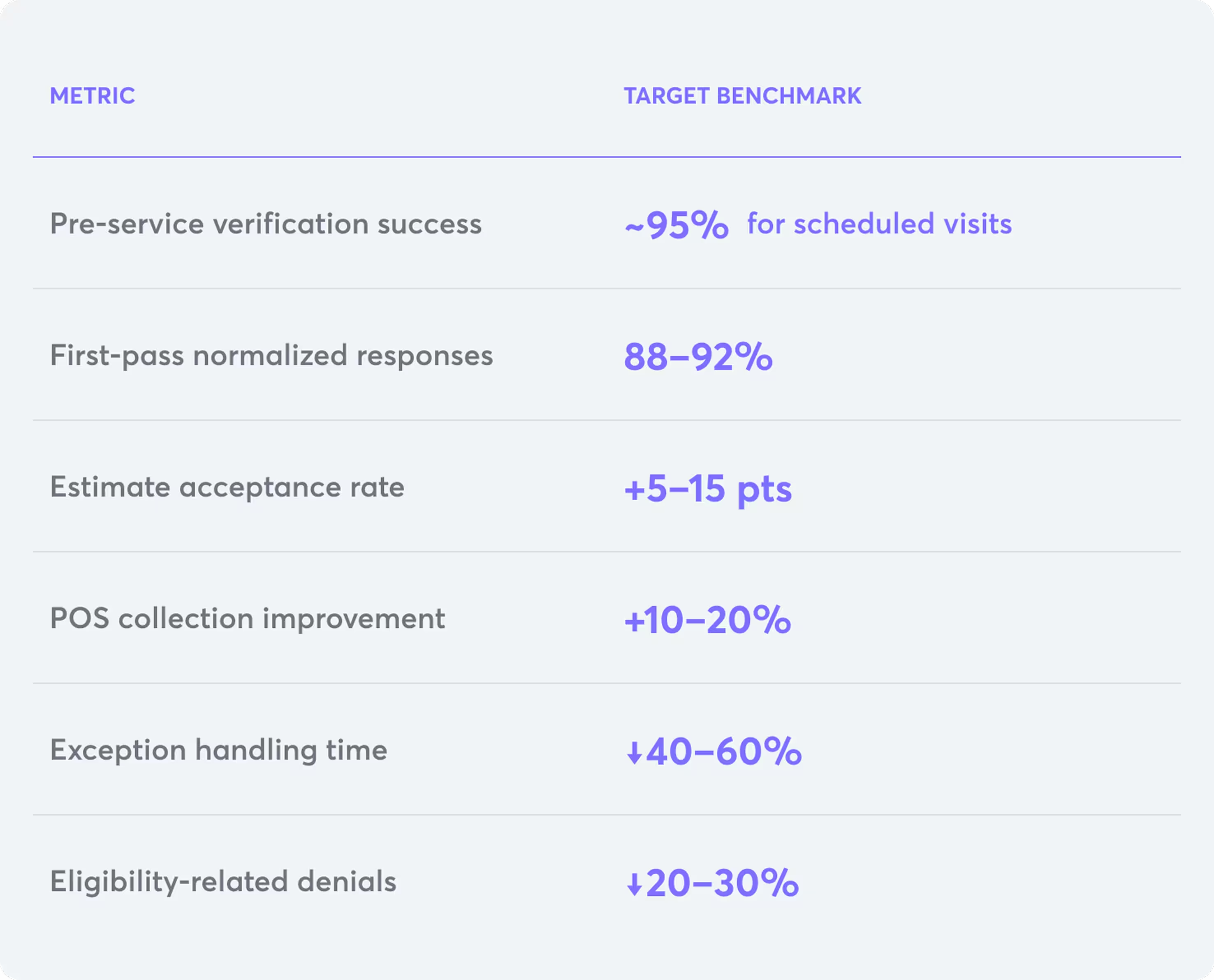
Measurable Outcomes
A scheduler books a visit; the AI agent verifies eligibility in seconds, builds a trustworthy estimate, and politely nudges the patient with a plain English summary and a one-tap way to pay or set a plan. Two days before the appointment, the system rechecks benefits; if the deductible just reset, it refreshes the estimate and sends an update so there are no desk-side surprises. If the payer’s response is thin, it augments via API; if an auth flag appears, it alerts the right queue before the day of service. When the claim leaves, scrubbing already “knows” the plan’s quirks, so you see fewer avoidable edits. This means:
- Pre-service medical insurance eligibility verification moves toward ~95% for scheduled services.
- First-pass eligibility success (complete, normalized responses) climbs into the high-80s to 90%+.
- Estimate acceptance ticks up 5–15 points with plain-language summaries and portal-optional payment.
- POS collection rate rises steadily month over month as friction drops.
- Exception average handling time (AHT) falls because packets arrive pre-digested.
- Eligibility-related denials trend down quarter over quarter; first-pass yield trends up.
And staff are sent exceptions with context; rather than navigating portals, PDFs, and decision fatigue, they have clear steps to obtain verification.
Implementation Quick-Start
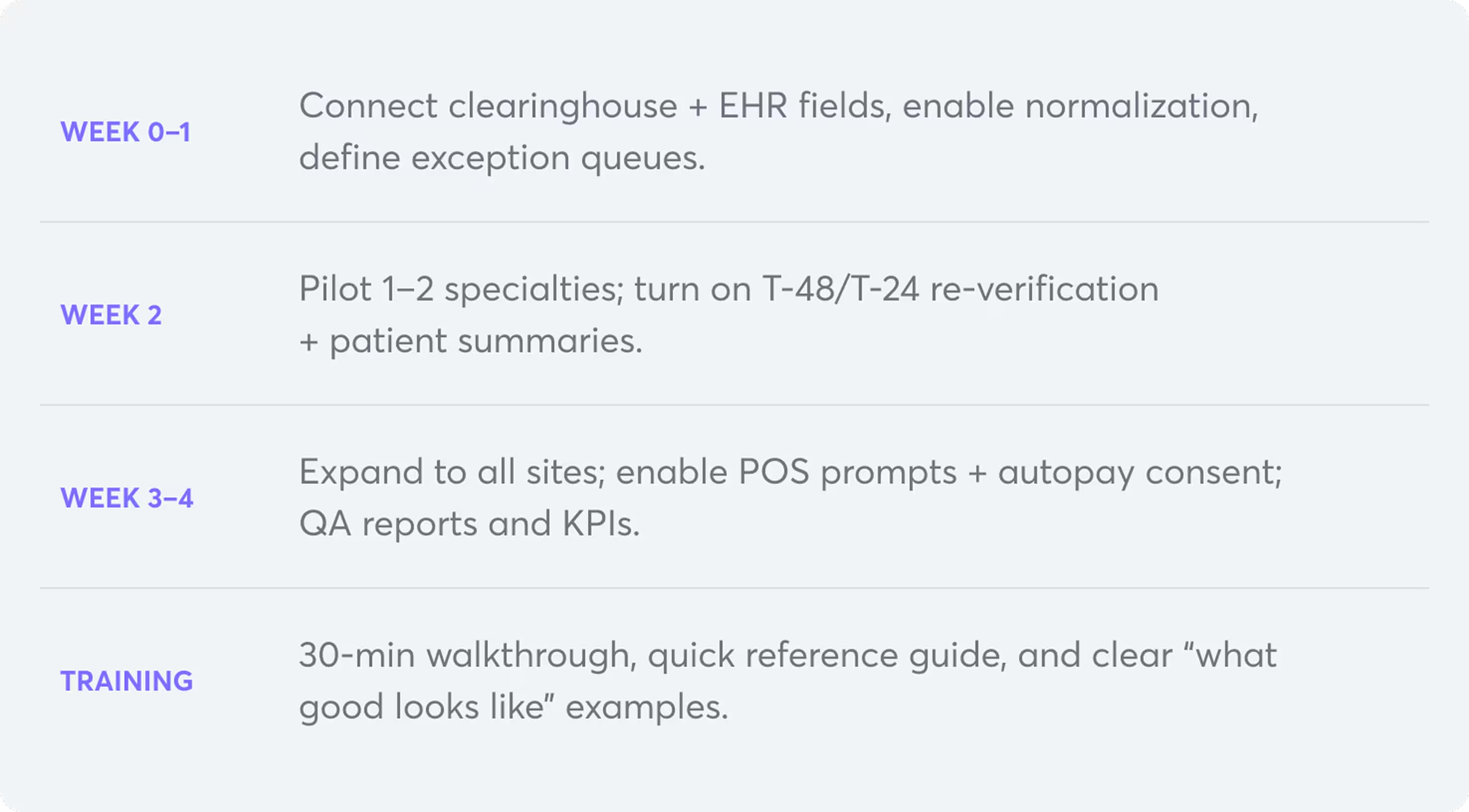
Tip: Keep Contact Info Current at Check-In
Terminal capture confirms patient mobile and email during intake and automatically updates them in the EHR. This ensures reminders, estimates, and receipts reach patients directly — no more “wrong number” loops.
Collectly’s AI for eligibility verification & co-pays
Collectly’s Billie AI Agent for Eligibility & Benefits automates real-time eligibility, normalizes clearinghouse responses into a structured format directly in your EHR, and instantly calculates patient-specific copays -- then carries that single, trustworthy signal through estimates and point-of-sale. This means faster cash, fewer surprises, and staff dedicated to people, not portals.
Agentic AI eligibility is a critical part of Collectly’s end-to-end, AI RCM and patient engagement platform:
- Pre-service: AI eligibility, and accurate cost estimates -- refreshed automatically at scheduling.
- Point of service: Seamless in-person and digital payments, portal-optional one-tap pay, and 60-second plans.
- Post-service: Automated billing, omnichannel follow-ups, and Billie Voice, our AI agent for patient billing support that resolves ~85% of billing questions so your team handles only true exceptions.
Relieve your team of heavy revenue cycle burdens like eligibility, A/R follow-up, and patient billing support while accelerating cash flow, reducing cost-to-collect, and delivering a patient-friendly financial experience. Schedule a demo today.















%20Workflows%20for%20Healthcare%20Providers%20.avif)
%20101.avif)
%20Glossary%20of%20Terms.avif)

%20for%20Healthcare%20%E2%80%A8Finance%20Teams.webp)



















