2025 Policy Changes: How the Law Will Impact Healthcare Revenue and Operations

On July 4, 2025, the federal budget reconciliation bill -- previously known as the "One Big Beautiful Bill Act" -- was signed into law. The provisions in this law, which roll out over the next five years, will reshape Medicaid, Medicare, and the Affordable Care Act marketplace programs across the U.S.
For healthcare providers, this law presents both short-term operational challenges and long-term, structural shifts in revenue streams. Upcoming changes, like the expiration of ACA premium tax credits and the addition of Medicaid work requirements, will increase the number of uninsured patients, the amount of bad debt, and the level of charity care needed. More frequent eligibility redeterminations and new verification requirements will increase the administrative burden -- and the potential for operational disruption -- for healthcare organizations.
While some provisions offer temporary relief, like a one-year 2.5% Medicare physician fee schedule increase, health organizations should prepare for an overall reimbursement environment that is more challenging and constrained than before. To stay afloat in these new waters, and even thrive, providers need to focus on how to accelerate cash flow, streamline RCM workflows, and improve the patient financial experience.
How Does the 2025 Budget Reconciliation Law Affect Medicaid?
The 2025 federal budget reconciliation bill brings significant changes to Medicaid, which covered 72 million people as of October 2024. This law introduces work requirements, restricts supplemental payments, and reduces Medicaid spending by nearly $1 trillion by 2034.
The effects of these changes will look different in each state, and healthcare providers operating under Medicaid expansion -- i.e. the 40 states and D.C. that expanded state Medicaid programs after the passage of the ACA -- will feel these funding cuts the most.
Here are the biggest changes coming to Medicaid:
New Work Requirements
- Before this law: Medicaid eligibility could be based on income alone, and many expansion states had no work requirements. An estimated 64% of Medicaid enrollees are working full-time or part-time jobs.
- After this law: Medicaid has mandatory work requirements for adults ages 19-64 starting Jan. 1, 2027. This requires 80 hours per month of employment or another qualifying activity to be eligible for Medicaid expansion coverage. Certain groups are exempted under this federal law, including parents of dependent children under age 14. States have discretion to set their own “look back” periods to verify employment, so enrollees who move to or work in another state will need to understand each state’s verification system and reporting requirements.
- Impact: Work requirements will cause the disenrollment of many Medicaid recipients, many of whom are eligible for Medicaid benefits but do not keep up with communication or documentation requirements. Administering this system will require complex system changes, which can cost hundreds of millions of dollars per state.
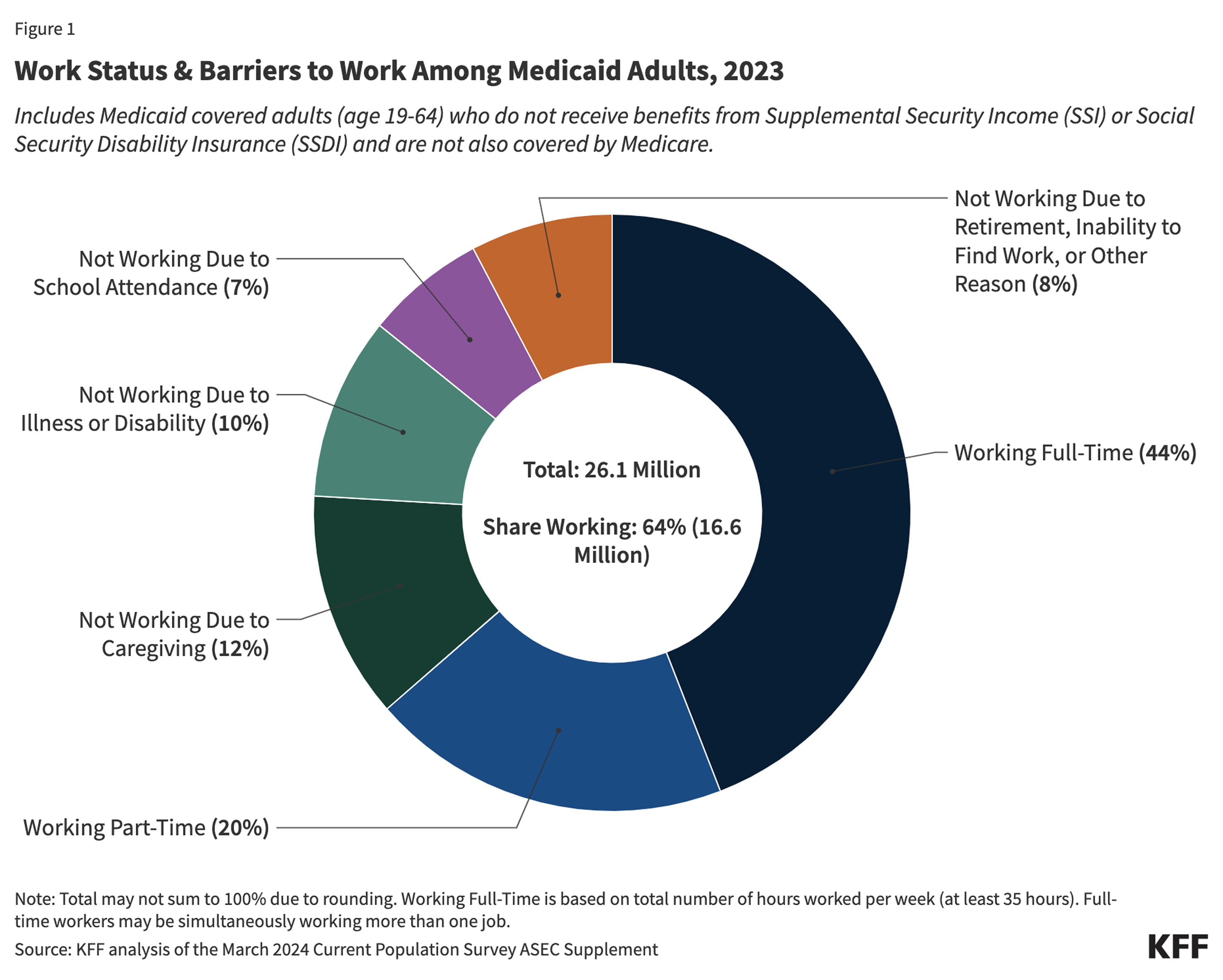
Image source: KFF -- 5 Key Facts About Medicaid Work Requirements
Decrease in Federal Reimbursements
- Before this law: Many hospitals operate at slim or negative margins, and Medicaid base payment rates are below the rates for Medicare or commercial insurance. States use federal matching funds and supplemental payment structures to help make up the shortfall, e.g. Disproportionate Share Hospital (DSH) payments and State-Directed Payments (SDPs).
- After this law: There are new caps and restrictions on supplemental payments. SDPs for inpatient hospital and nursing facility services are capped at 100% of the Medicare payment rate for expansion states and at 110% for non-expansion states starting in 2025, and existing payments above those levels will be reduced starting in 2028.
- Impact: With $149 billion less Medicaid funding over 10 years, states will need to drastically cut Medicaid programs and/or other parts of the state budget. This will affect almost all health organizations, but especially providers in expansion states with a high rate of Medicaid patients.
“Without SDPs, Medicaid managed care payments to hospitals would be less than half of the rate paid by other payers, which is not enough to sustain access to the essential services that hospitals provide, such as maternity, trauma, and behavioral health care.”
Source: Essential Hospitals -- Policy Brief: How State Directed Payments Support Hospitals
More Frequent Eligibility Checks
- Before this law: Medicaid recipients undergo eligibility verification annually.
- After this law: States must reverify the eligibility of Medicaid expansion adults twice annually, starting with renewals scheduled on or after Dec. 31, 2026.
- Impact: More frequent verification leads to coverage lapses and coverage terminations for many, especially those lacking stable employment or reliable access to documentation. It also adds to the administrative burden for states, many of which are already stretched thin to administer state Medicaid programs. For example, even before the 2025 federal budget reconciliation law, unexpected delays in supplemental Medicaid payments caused health organizations to lay off staff and close facilities. Massive reductions in supplemental payments, plus new administrative burdens on states, will have compounding effects on providers’ revenue.
Reduced State Medicaid Budgets
- Before this law: The joint federal-state financing model allowed flexibility for funding healthcare operations, especially in expansion states.
- After this law: With federal cuts and structural changes, states will lose $1.2 trillion in Medicaid funding over 10 years, with most of those reductions in expansion states. (For example, the state of Kentucky faces an estimated decrease of $12+ billion over 10 years.) In addition, states are prohibited from increasing existing provider taxes or adding new provider taxes as of 2025.
- Impact: Many states will need to reduce their provider taxes to comply with new regulations. States must cut services, reduce eligibility, or decrease provider reimbursement rates to make up for the reduction in federal funding. These changes will have a ripple effect across all healthcare organizations.

Image source: KFF -- 5 Key Facts About Medicaid and Provider Taxes
Cuts to Rural Health Systems
- Before this law: There are nearly 1,800 rural hospitals in the U.S., and they rely heavily on Medicaid funding to stay open. Medicaid covers ~40% of children and nearly half of all births in rural areas.
- After this law: Rural providers will lose significant Medicaid funding over the next 10 years, with estimates ranging from $70 billion to $137 billion over 10 years. The Rural Health Transformation Program adds $50 billion to rural healthcare to offset massive cuts, but it’s not yet clear how funds will be distributed, what criteria the Centers for Medicare and Medicaid Services (CMS) will use to approve or deny applications, or whether funds will be directed to certain types of rural providers.
- Impact: Rural hospitals are already more likely to be operating on negative margins (44%) than urban hospitals (35%). Rural facilities tend to be smaller sites with lower patient volume, and they may not be equipped to offer specialized care that delivers higher reimbursement rates. These changes will strain rural providers, putting 400+ rural hospitals at risk of closure. The continued closure of rural healthcare sites severely reduces access to maternal, trauma, and behavioral health care -- especially in Medicaid expansion states with a large percentage of rural children covered by Medicaid, such as New Mexico, Louisiana, Arizona, and Arkansas.
“Currently, even with ten regional offices, Rural Health Clinics (RHC) often experience significant delays in receiving their billing numbers after passing the necessary surveys. These delays are not just a matter of inconvenience -- they pose a critical financial burden. Delaying the functional and billing operations of potential RHCs will constrict access to care for residents of rural areas. Each day of delay compounds financial strain, pushing some clinics to the brink of closure.”
Source: National Rural Health Association -- Rural Health Implications for Reorganization of HHS Regional Offices
How Does the Law Affect ACA Marketplace Plans?
- Before this law: For the 24 million-plus Americans on ACA marketplace plans, enhanced subsidies passed in 2021 help enrollees afford healthcare coverage. This is especially important in non-Medicaid expansion states, where a higher percentage of residents rely on marketplace plans (and subsidies) for affordable coverage. These enhanced subsidies will lapse at the end of December 2025, making it harder for enrollees to pay for coverage. Compounding the issue, insurers in several states plan to increase rates for 2026 marketplace plans -- public rate filings show a requested premium increase of about 15%, the steepest since 2018.
- After this law: The ACA subsidies approved in 2021 will be rolled back January 1, 2026. Enrollees will see higher premiums in 2025 and fewer subsidies to help pay for their healthcare costs. Starting in January 2027 (or earlier at state request), people who are denied or disenrolled from Medicaid due to work requirements will be ineligible for subsidized ACA plans.
- Impact: ACA enrollees receiving subsidies will experience a significant increase in out-of-pocket premium costs when these subsidies expire. Increased costs, plus stricter enrollment and eligibility requirements, will put an estimated 8.2 million enrollees in coverage limbo. With millions losing ACA coverage due to shrinking subsidies and/or tighter signup requirements, people who stay in marketplace plans are likely to be less healthy and have higher claims costs on average; this leads insurers to further increase premiums to cover the changing insurance pool, and the cycle continues.
The Bottom Line for Healthcare Providers
The unwinding of continuous enrollment, plus new eligibility requirements and stricter reverification processes, will cause an estimated 8.7 people to lose Medicaid coverage, and millions more to lapse or lose ACA coverage. As a result, healthcare providers must brace for a sharp increase in uncompensated care and a major decrease in state and federal funding support.
“It is a double-whammy. We're going to have many millions more uninsured individuals showing up needing care, but at the same time, hospitals won't be able to backfill financial holes.”
Source: Wall Street Journal -- How Healthcare Cuts in the 'Big, Beautiful Bill' Will Affect Americans
With fewer funds available and new restrictions on supplemental payments, the financial situation looks dire -- especially for rural providers and safety-net hospitals. As out-of-pocket patient costs go up, patient collection rates tend to go down. To stay financially viable, healthcare providers need to prioritize operational solutions:
- RCM Process Automation -- use automation and AI to make RCM workflows more accurate, more efficient, and easier to execute
- Boost A/R Management -- reduce your days in A/R and bad debt rate with simple billing statements and digital billing tools that make it as easy as possible for patients to pay
- Better Patient Intake -- increase prepayment and point-of-service collections with a streamlined patient intake process
- More Consistent Patient Communication -- set accurate patient expectations upfront and automate billing and payment reminders
- Offer Patient Billing Support -- offer self-service payment plans and use an AI agent for 24/7 patient billing support to help patients navigate outstanding balances
These 2025 policies and expected rising patient responsibility will squeeze practice margins. Protect them now with Collectly’s AI RCM and patient billing: pre-service check-in and cost visibility, modern self-service payments, and automated post-visit outreach that adapts in real time.
Billie, our AI agent, answers billing questions 24/7 across chat, SMS, email, and voice -- clearing confusion and accelerating payments without adding headcount. Native EHR integrations, real-time analytics, and flexible payment plans help you improve cash flow and reduce cost to collect -- fast. Learn more here.















%20Workflows%20for%20Healthcare%20Providers%20.avif)
%20101.avif)
%20Glossary%20of%20Terms.avif)

%20for%20Healthcare%20%E2%80%A8Finance%20Teams.webp)



















